[smbtoolbar]
Understanding the importance of the GMFCS, a group of doctors, professor, OTs and PT in Sweden developed the Manual Ability Classification System (MACS) “to classify how children with cerebral palsy use their hands to handle objects in daily life.” (www.macs.nu)
The MACS has 5 levels:
- Handles objects easily and successfully.
- Handles most objects but with somewhat reduced quality and/or speed of achievement.
- Handles objects with difficulty; needs help to prepare and/or modify activities.
- Handles a limited selection of easily managed objects in adapted situations.
- Does not handle objects and has severely limited ability to perform even simple actions.
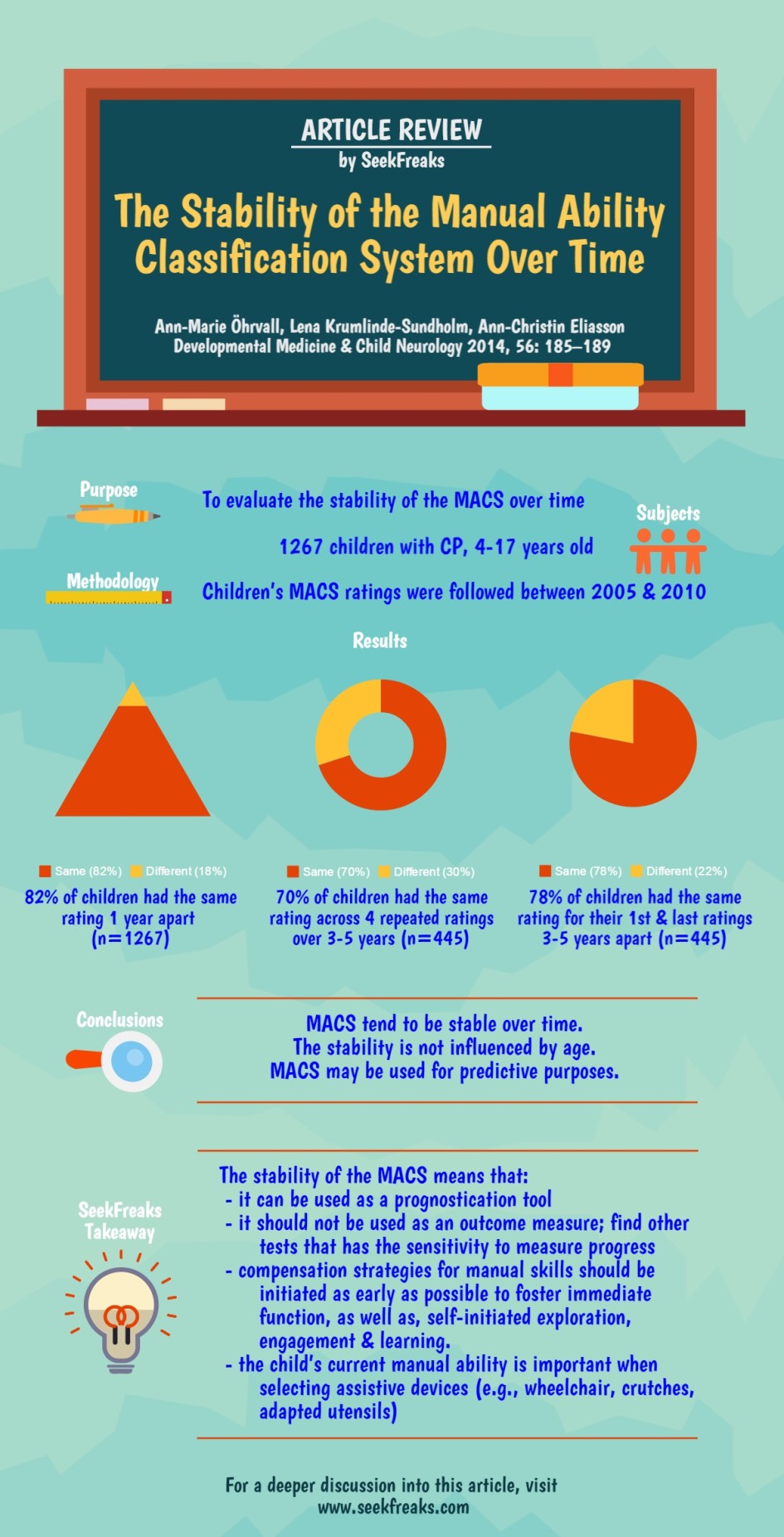
The recent “Scoping Review of the MACS” published in the Fall 2015 Pediatric Physical Therapy Journal has inspired me to revisit this MACS stability study published in 2014. In the latter study, Öhrvall et al demonstrated that:
- The MACS is stable in 70% of children with CP, 4-17 years old, across repeated ratings followed for 3-5 years between 2005-2010;
- Stability is even higher, at 78%, if you only look at the 1st and last ratings between those 3-5 years
- Discrepancies in MACS rating occurred mostly (122 of 133) 1 level higher or lower than the previous rating, with no systematic movement up or down (i.e., it went up almost just as much as it went down).
- Levels I and V are the most stable, perhaps because there is only 1 direction for movement in these levels.
The study gave 2 reasons for the stability:
- Broadness of each MACS categories
- Age-related development is built in to the MACS (i.e., the handling always refer to age-appropriate objects).
For sure, this was sobering news, similar to the initial discovery of the stability of the GMFCS. Since MACS is a measure of children with cerebral palsy’s “ability to handle objects in daily life” (www.macs.nu), this means that children at age 4 will likely have the same ability to handle objects when they reach 17, and that therapeutic interventions that focus on remediating the child’s body function will likely result in no change in MACS levels.
However, having this knowledge of prognostication is also great news! In the schools, we can work with the teachers and the IEP team to modify expectations. We can also employ more effective interventions that can improve a child’s participation and activity level with less emphasis on treating the child’s impairment directly. Interventions that focus on compensation such as modification of the task or environment, and introduction of assistive technology should begin as soon as possible. This may help promote self-initiated exploration and engagement, just as the early introduction of wheelchairs to young children with lower GMFCS Levels has done.
The authors warn that the MACS should not be used as an outcome measure. This makes sense when you consider its stability. Other tests should be selected if you would like sufficient sensitivity to measure progress resulting from intervention.
It would be interesting to find out whether the MACS will become as influential in prognostication as the GMFCS has been. Perhaps, more articles needs to be published both on its application in research and clinical practice. Studies that span more than 5 years is also needed to further establish longitudinal stability. Other questions that may need to be answered include: what could cause changes in MACS levels? Are there special procedures (e.g., botox injection, surgery, constraint induced movement therapy, etc.) that can result in increasing MACS level?
Finally, I would caution those of us tempted to see 70% as too low and hang their hopes on the 30% of the children whose MACS levels have changed over time. As mentioned, changes were almost as frequently down as they are up. Moreover, even if one decides to continue remediation strategies, it should not preclude the concurrent use of compensatory strategies that would help the child gain immediate function.
~~~~~~~~~~ 0 ~~~~~~~~~~
Freakishly Fast Poll:
~~~~~~~~~~ 0 ~~~~~~~~~~
Seeking Your Views:
Do you think the MACS is useful for your school-based practice?
How have you applied it or how would you apply it?
Who else needs to hear about the results of this study?
Leave your answers and comments below.
~~~~~~~~~~ 0 ~~~~~~~~~~
Readers of this article also read these:
Functional Classification Systems for Children with CP
Motoropoly 3: Motor Learning Principles in School – Salience, Frequency, & Whole vs. Part Practice
50 Alternatives to “Good Job!”
Late Summer Reading List for Seasoned School-based OTs, PTs and SLPs