[smbtoolbar]
It has been a difficult political year. How about something on which we can ALL agree? Medicaid, specifically Medicaid in education! I don’t know of anyone who is a fan of this pairing. So how about a few basic questions and answers to begin a discussion of this awkward funding source for special education and related services. I know there are strong opinions about this topic, so let’s set high expectations for civility, SeekFreaks!
Please note this information is provided for general informational purposes. You must verify information for your state as each state has a State Medicaid Plan which can vary widely. Here we go…
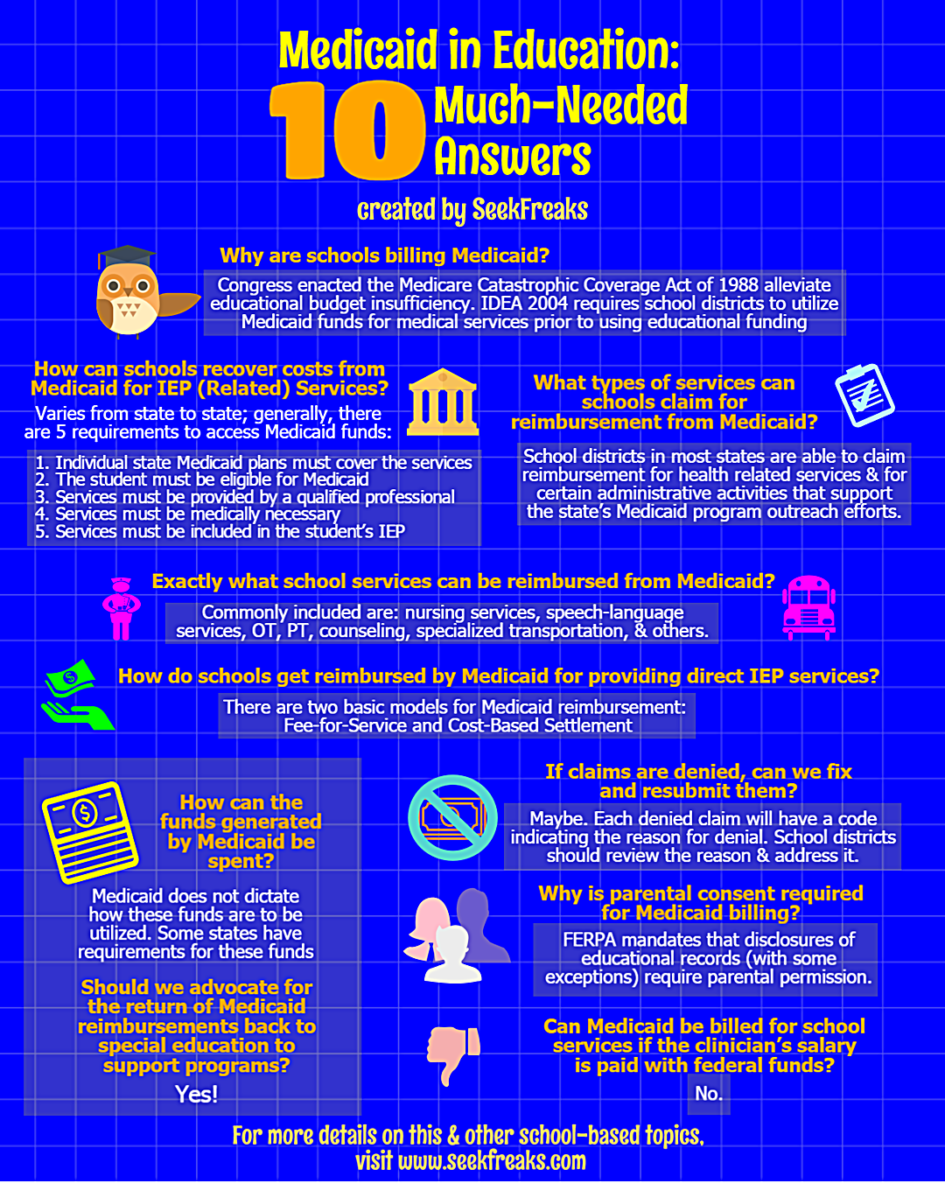
Question 1. Why are schools billing Medicaid?
The Individuals with Disabilities Education Act (IDEA) mandates state and local educational efforts for students with disabilities. When IDEA was enacted, the federal government contribution to special education was targeted to reach 40 percent of the estimated cost of educating students with disabilities for 1982 and every subsequent year. Federal funding of special education has fluctuated between 14-18% on average. Congress recognized this funding shortfall and attempted to alleviate educational budget insufficiency by enacting the Medicare Catastrophic Coverage Act of 1988 (P.L. 100-360). This legislation established a financial relationship between IDEA and Medicaid, encouraging school districts to recover costs for medical services from Medicaid.
Further, IDEA 2004 [Title I B 612a12A(i)] actually requires school districts to utilize Medicaid funds for medical services prior to using educational funding. Here is the actual citation:
(i) Agency financial responsibility.–An identification of, or a method for defining, the financial responsibility of each agency for providing services described in subparagraph (B)(i) to ensure a free appropriate public education to children with disabilities, provided that the financial responsibility of each public agency described in subparagraph (B), including the State Medicaid agency and other public insurers of children with disabilities, shall precede the financial responsibility of the local educational agency (or the State agency responsible for developing the child’s IEP.)
Here is relevant language from the Centers for Medicare & Medicaid Services 2003 Administrative Claiming guide:
IDEA-related health services. The Individuals with Disabilities Education Act (IDEA) was passed to “assure that all children with disabilities have available to them… a free appropriate public education which emphasizes special education and related services designed to meet their individual needs.” The IDEA authorizes federal funding to states for medical services provided to children through a child’s Individualized Education Program (IEP), including children that are covered under Medicaid. In 1988, section 1903(c) of the Act was amended to permit Medicaid payment for medical services provided to Medicaid eligible children under IDEA and included in the child’s IEP.
School districts cannot ‘make’ money from Medicaid reimbursement. Districts recover cost of mandated (and expensive) services and personnel. Medicaid now requires each district to submit a cost report which specifies how much was spent on services for students and how much they received from Medicaid. If they received more than they spent, they must return the difference; Medicaid eventually returns the difference if the district spent more than they received. It is a zero sum game.
Question 2: How can schools recover costs from Medicaid for IEP (Related) Services?
Requirements may vary from state to state. All requirements are described in the State Medicaid Plan for each state. Generally speaking, there are five requirements for public schools to access Medicaid funds:
- Individual state Medicaid plans must cover the services
- The student must be eligible for Medicaid
- Services must be provided by a qualified professional within the scope of their practice
- Services must be medically necessary
- Services must be included in the student’s IEP – While many state plans still require that reimbursed services are included in an IEP; the Centers for Medicare and Medicaid (the feds) have reversed this expectation. Inclusion of services in an IEP is no longer required by CMS but state plans must open to remove this language and be approved. Therefore is it likely this will continue to be required by states, at least for a time.
If these conditions are met, schools may be reimbursed from Medicaid funds for medical services as described in each state’s Medicaid plan. In most cases, this requires that school districts or Local Education Agencies (LEAs) become Medicaid providers and follow the state Medicaid agency’s requirements for processing claims for reimbursement.
Question 3: What types of services can schools claim for reimbursement from Medicaid?
There are two basic types of services that Medicaid reimburses for public schools. School districts in most states are able to claim reimbursement for health related services they provide to Medicaid eligible students and for certain administrative activities that support the state’s Medicaid program outreach efforts. These are separate but related reimbursement programs; states have specific requirements for each program.
- Direct Service Claiming for IEP (Related) Services: Direct service claiming is a program that reimburses school agencies for providing direct health related services to Medicaid eligible students. The services are identified within a student’s Individual Education Program (IEP) or Individualized Family Service Plan (IFSP) and are delivered as a component of the agency’s special education services. The direct health related services (e.g. nursing, various therapies) are routinely performed by school employees and contracted staff in a school setting. Eligible services varies from state to state according to each State Medicaid Plan.
- Administrative Claiming: Administrative Claiming (Medicaid Administrative Claiming, School Based Administrative Claiming, Administrative Claiming for Education) is a program that reimburses school agencies for activities that help families understand Medicaid programs and services they may need as well as eligibility information. Activities could include scheduling and/or coordinating medical screens or mental health diagnostic services, coordinating a meeting with school staff and parents to determine if mental health or educational evaluations are needed. The administrative activities are routinely performed by school employees and/or contracted staff in the school setting.
Additional Services may be billable under Early Periodic Screening, Diagnosis and Treatment (EPSDT). Please check your Medicaid State Plan.
Question 4: Exactly what school services can be reimbursed from Medicaid?
The services that can be reimbursed by Medicaid are described in each state’s State Medicaid Plan, specific services can vary from state to state. Services that are commonly included are: nursing services, speech-language services, occupational therapy, physical therapy, counseling, specialized transportation, among others.
Question 5: How do schools get reimbursed by Medicaid for providing direct IEP (related) services?
There are two basic models for Medicaid to reimburse services schools provide:
- Fee for Service (FFS): In this reimbursement model, the state establishes the Medicaid reimbursement rate for each billable service provided by the school agency. The school agency is reimbursed at the set rate for every service it provides regardless of its cost to provide the service. A school district can receive reimbursement for every Medicaid eligible service that is documented on the IEP or IFSP to support the education of a Medicaid eligible student. The amount of federal reimbursement for each reimbursed service varies by state. Reimbursement rates are set by each state, based on the following:
- the cost of providing the service,
- review of reimbursement rates by private payers,
- federal matching formulas (more on federal match in the next issue!) and
- a percentage of what Medicare pays for equivalent services.
- Cost-Based Settlement: In this reimbursement model, school agencies receive periodic “interim” payments during the school year from the state Medicaid agency. These interim payments reimburse the school agency for providing the required school Medicaid services. At the end of a State Fiscal Year, school agencies calculate the total costs they incurred to deliver the services. The agency’s actual costs are then compared to the total interim payments paid during the fiscal year. If the total allowable actual costs are greater than the interim payments made, there is an additional settlement reimbursement made to the school district. If the total allowable costs are less than interim payments made, the difference is recaptured by the Medicaid agency.
Question 6: Can Medicaid be billed for school services if the clinician’s salary is paid with federal funds?
No. If the clinician salary is paid with federal education funding, services they provide should not be submitted for cost recovery as this would be ‘double-dipping,’ e.g., utilizing federal funds to generate federal funds.
Question 7: How can the funds generated by Medicaid be spent?
Medicaid does not dictate how these funds are to be utilized. This can vary state to state and even school district to school district. Some states have requirements for these funds, others leave how to spend the Medicaid reimbursements to the local districts (and everything in between!).
Question 8: Should we advocate for the return of Medicaid reimbursements back to special education to support programs?
Yes! The Medicare Catastrophic Coverage Act of 1988 (P.L. 100-360) was intended to address the shortfall in funding IDEA. Medicaid reimbursements should be utilized for special education and related services.
Question 9: If claims are denied, can we fix and resubmit them?
Maybe. Each denied claim will have a code indicating the reason for denial. School districts should review the reason it was denied and if possible submit additional documentation or records to verify the claim. If there is an outright error, claims should not be fixed or altered in any way for resubmission; just re-pay the amount of the claim.
Question 10: Why is parental consent required for Medicaid billing?
Records maintained by a School Agency regarding the provision of special education services (including medical services such as speech therapy, counseling, nursing services, etc.) are classified as “educational records”. Disclosure of educational records is covered by the Federal Educational Rights and Privacy Act (FERPA).
FERPA mandates that disclosures of educational records (with some exceptions) require parental permission. Sending information about medical services for students to the State Medicaid Agency is classified as a disclosure of educational records and so requires parental consent (or consent of the student if he/she has reached the age of majority).
And now…BONUS INFO! A great resource: The National Alliance of Medicaid in Education (NAME)
The National Alliance for Medicaid in Education, Inc. (NAME) is a non-profit 501(c) (3) organization comprised of members from the nation’s school districts, state Medicaid and Education agencies, businesses, consulting firms, non-profit organizations, and federal agencies who are involved in administration of Medicaid claiming for school-based services.
NAME provides information about national and state Medicaid policy and practices that affect school Medicaid claiming. A quarterly newsletter that covers national and regional news, national topical calls, school-based Medicaid biennial survey, and current information are just a few resources that can be found on the NAME website.
Three main purposes drive NAME’s services to its members:
- Provide leadership
- Promote integrity, collaboration and success
- Facilitate a network to share information
NAME strives to provide a forum for members to network and exchange information on all areas of school Medicaid. Other benefits to members include:
- Annual conference and meeting
- Quarterly newsletter
- Members-only section of the NAME website devoted to providing resources
- National teleconference sessions – at least two per year
- Regular interaction with federal partners such as CMS and USDOE/OSEP
- National partners with similar missions such as AASA, NASDSE, CASE, NAMD, etc.
For more information on NAME resources or membership, go to: http://www.medicaidforeducation.org
~~~~~~~~~~ 0 ~~~~~~~~~~
Readers of this article, also read these:
Top 10 Walking Tests for School-based Therapists
Call to Action: Full Funding of IDEA










1 Pingback