[smbtoolbar]
Although we often talk about functional tests here at SeekFreaks, it is also important to look at impairment level tests. Results of such tests can often help identify the cause of activity limitations and participation restrictions (see Recognizing ICF Domain Words…Amusing Musings). They can also be very useful in designing intervention plans.
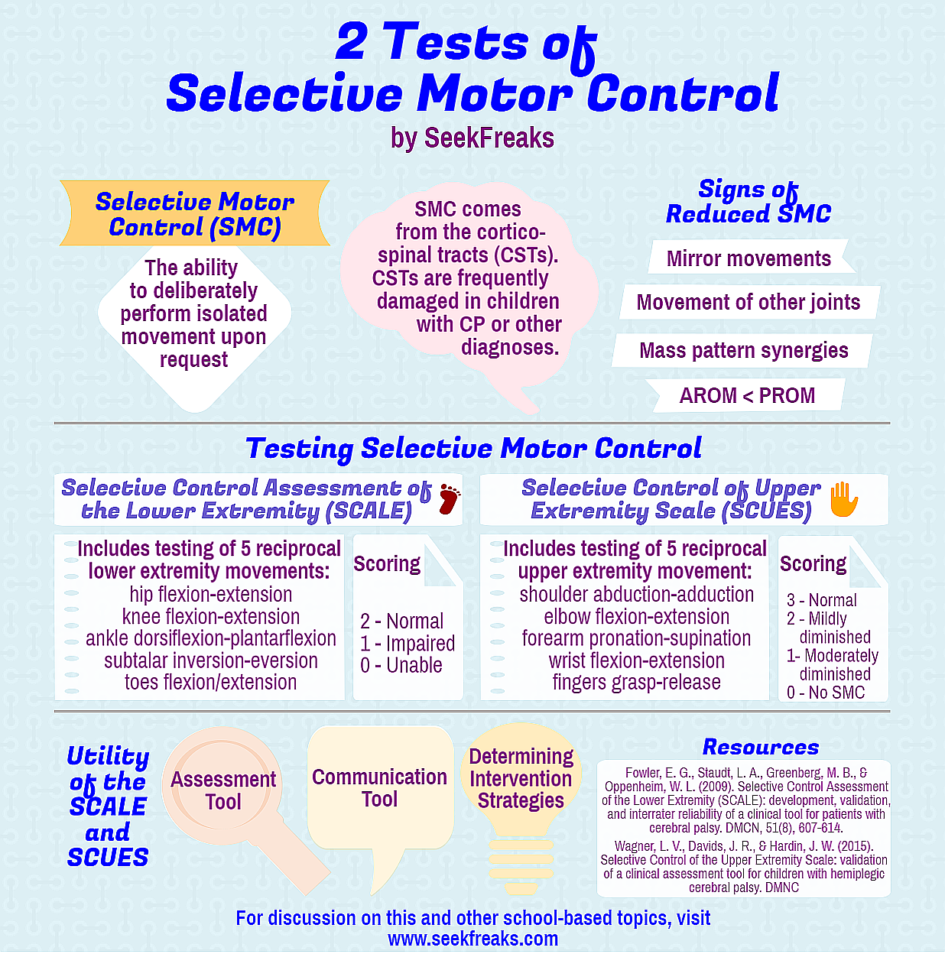
Cahil-Rowley & Rose (2014) listed 4 inter-related neuromuscular deficits for spastic Cerebral Palsy (CP) as muscle weakness, spasticity, short muscle-tendon length and selective motor control. While there are many ways to measure the first 3 easily (muscle testing, range of motion, Tardieu scale for spasticity, etc.), until recently, the latter was only measured via electromyography. For this article, we will look at 2 standardized assessments for selective motor control that can be administered easily, cheaply and quickly.
Selective Motor Control (SMC) [aka Selective Voluntary Motor Control (SVMC)] is defined as the “deliberate performance of isolated movement upon request,” which is different from “habitual selective muscle activation during functional tasks, such as walking” (Fowler et al, 2009). Why should we look at SMC? Voorman, et al (2007) found SMC to be the most important factor in determining gross motor function amongst other factors they studied (such as range of motion, muscle strength, spasticity, etc.). SMC comes from the cortico-spinal tracts (CST), which originated in the cortex (hence the name). CSTs are frequently damaged in children with Cerebral Palsy and other diagnoses. When an individual whose CST is damaged is asked to perform an isolated movement, a reduced SMC can be observed as:
- Movement of joints other than the one being tested (shoulder flexes when asked to flex the elbow)
- Mirror movements (both elbow flexes when asked to bend one elbow)
- Mass pattern movement (aka as synergies)
- Active range of motion (AROM) is less than passive range of motion (PROM)
Cahil-Rowley & Rose (2014) provides a great discussion on why the above occur when the CST is damaged in children with CP. They speculate that the rubrospinal tract (RST), which originates in the brainstem, provides an imperfect compensation for the functions of the CST.
Standardized Assessment of Selective Motor Control
So, is there a standardized way of assessing SMC? Luckily, there is not 1, but 2 that we will discuss: the Selective Control Assessment of the Lower Extremity (SCALE) and the more recently published Selective Control of Upper Extremity Scale (SCUES). As a great bonus, these tests are free and take no more than 15 minutes to administer each.
Here are some resources to get you started:
- SCALE (Fowler et al, 2009)
- SCUES (Wagner et al, 2015)
Testing and Scoring
The SCALE includes testing of 5 reciprocal lower extremity (LE) movements: hip flexion-extension, knee flexion-extension, ankle dorsiflexion-plantarflexion, subtalar inversion-eversion, and toe flexion/extension. While the hip test is performed in sidelying, the other 4 tests are done in sitting. The tester 1st passively moves the limb “through the desired movement sequence using a three-second verbal cadence” (Fowler et al, 2009).
Each LE is tested separately, watching out for the ability to move a joint selectively, and other extraneous movements or signs of reduced SMC as described earlier. Each movement is graded in a scale of 0-2:
- 2 or Normal – when the movement is completed within 3-second cadence and without extraneous movements
- 1 or Impaired – when isolated movement occurs for part of the task, but any of the following occurs:
- Extraneous movement from other body parts (including mirroring)
- Movement of tested part only towards 1 direction (e.g., extension, but not flexion)
- AROM is less than 50% of PROM
- Movement exceeds 3-second cadence
- 0 or Unable – when movement is not initiated, or when the individual uses synergistic mass movement pattern
Scores for each limb is added up for a perfect score of 10 out of 10.
The SCUES includes testing 5 reciprocal upper extremity (UE) movements: shoulder abduction-adduction, elbow flexion-extension, forearm pronation-supination, wrist flexion-extension, and fingers grasp-release. All tests are performed in sitting. Each UE is tested separately, watching out for the ability to move a joint selectively, and other extraneous movements or signs of reduced SMC as described earlier. The child’s performance is videotaped, which the tester watches and scores. Each movement is graded from 0-3:
- 3 is Normal SMC
- 2 is Mildly Diminished SMC
- 1 is Moderately Diminished SMC
- 0 is no SMC
The scoring of SCUES is more complicated compared to the SCALE, so I refer you to the Directions for Scoring.
Both tests have been shown to be valid and reliable. While both tests were designed for use with individuals with CP, Fowler, et al (2009) suggests that the SCALE may be useful for individuals with other neurological involvement. Note that Fowler, et al were able to test children with GMFCS Levels from I-IV. They were unable to test children with GMFCS Level V due to dyskinesia and/or inability to follow commands.
Research Using the SCALE
Below are a few things that research studies using the SCALE have shown. (Note that the SCUES is fairly new and has not been used in research as much as the SCALE.)
- Increased Distal SMC Impairment
Fowler, et al (2010) found “statistically significant decreases in SCALE scores from hip to toes.” Thus, they conclude that individuals assigned a score of 2 at the ankle are more likely to have scores of 2 at the knee and hip. This can be explained by the more medial somatotopic organization of distal LE CSTs compared to proximal LE CSTs; the former being more vulnerable to periventricular damage than the latter.
- SMC Is Predictive of Coordinated Movement during the Swing Phase of Gait
Fowler & Goldberg (2009) found that subjects with higher SCALE scores performed better during the portion of the gait cycle where hip flexion with simultaneous knee extension occurred. Not unexpectedly, those with lower SCALE scores had difficulty uncoupling hip flexion from knee flexion as they are not part of the same movement synergy.
- Prognostic Indicator for Hamstring Lengthening?
Goldberg, et al (2012) reported a case study with 2 patients who underwent hamstring lengthening. Subject 1 had SCALE scores of 2 (left) and 3 (right), while subject 2 had SCALE scores of 6 (left) and 5 (right). The authors found that subject 2 had greater stride length and faster walking speed after the surgery. So, hamstring lengthening seem to be more beneficial for patients with better SMC.
Utility of SCALE and SCUES
The latter finding above shows the potential of the SCALE and SCUES in determining realistic goals. So, how can the SCALE and SCUES be used in determining OT or PT interventions? Unfortunately, there are still many unknowns about SMC.
Although it seems that the SMC is stable pre- and post-hamstring lengthening, we do not yet know whether SCALE scores are stable in the long term despite any intervention. In short, we don’t know whether SMC can be improved? Cahil-Rowley & Rose (2014) also asks whether the RST can be trained to be a better compensator for the CST? If so, which interventions are helpful? More research is needed to answer these questions. I do hope there are researchers attempting to answer these questions using the SCALE and SCUES. Until then, here are some suggested uses for both tests:
- Assessment Tool
The SCALE and SCUES will definitely have a spot in my arsenal of assessments. When used together with other tests, they can help determine the cause of a participation restriction or activity limitation. Is it flexibility? Strength? Spasticity? Selective motor control? Something else? A combination of causes?
- Communication Tool
Being able to quantify the child’s SMC can help therapists communicate better to family, educators, and other stakeholders the probable cause of a child’s inability to participate or complete certain tasks. We now have more informed answers to questions like, why does he trip? Why is she having a hard time putting her jacket on? Or bringing the spoon to her mouth without spilling? Knowledge of a child’s SMC can also be put to good use when writing justification letters for ordering certain adaptive devices, and determining what kind of adaptive devices are needed.
- Deciding Intervention Strategies
Once the cause(s) are known comes the question of what combination of remediation and compensation strategies are you going to use. This is where knowledge of the tests’ long-term stability would have been very helpful. Should SMC be shown to be stable over time, more compensation strategies appear to be the better option. (Frankly, based on my own experiences, I’m leaning more towards compensation for children with low SCALE or SCUES scores). What compensatory strategies can I implement right away to help the child feed himself, get on those steep steps of the school bus, or complete his homework? If instead, one chooses more remediation strategies, the SCALES and SCUES can be conducted periodically to see whether the scores change. And if they don’t, you should stay focusing more on compensation.
Who has used the SCALE or SCUES? Share with us how you have used them.
~~~~~~~~~~ 0 ~~~~~~~~~~
Readers of this article also read these:
OTs, PTs & SLPs in Schools…How Did We Get Here?
50 Alternatives to “Good Job!”
4 Cs of Letters of Medical Necessity
10 Handy American Occupational Therapy Association Fact Sheets










March 29, 2017 at 10:27 am
Wow, this article was fantastic! Thank you!!
I looked into the SCALE measure earlier this year, as well, for one of the assessment projects I am working on. I am still always on the lookout for research in which the SCALE (or SCUES) is used as one of the outcome measures. There are hardly any right now! However, I did just recently come across one:
https://www.ncbi.nlm.nih.gov/pubmed/?term=Home-Based+Versus+Laboratory-Based+Robotic+Ankle
In this study, children (GMFCS 1-3) used a robotic ankle 3X per week over 6 weeks. The intervention consisted of 10 minutes
of passive stretching of the ankle, 20 minutes of active movement
training, followed by 10 minutes of passive stretching. They actually found that SCALE scores improved significantly in both the laboratory and home program groups (although only the laboratory group achieved the MDD of almost 2 scale points (according to Balser et al, 2016)). Disappointingly, another study replicated the ankle robot intervention with much smaller SCALE improvements seen. However, the intervention was done twice a week instead of 3x, so the intervention frequency was not identical.:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4112152/
Anyway, thanks again for this fabulous post!!
March 29, 2017 at 11:53 am
Thanks for this comment and references. I will definitely read them. By the way, there is one more SMC test for the upper extremity called TASC http://www.aacpdm.org/UserFiles/file/IC15-Staudt.pdf
January 3, 2021 at 11:28 am
Wondering if you are familiar with when you can start using the SCALE? What age would be appropriate/valid?