[smbtoolbar]
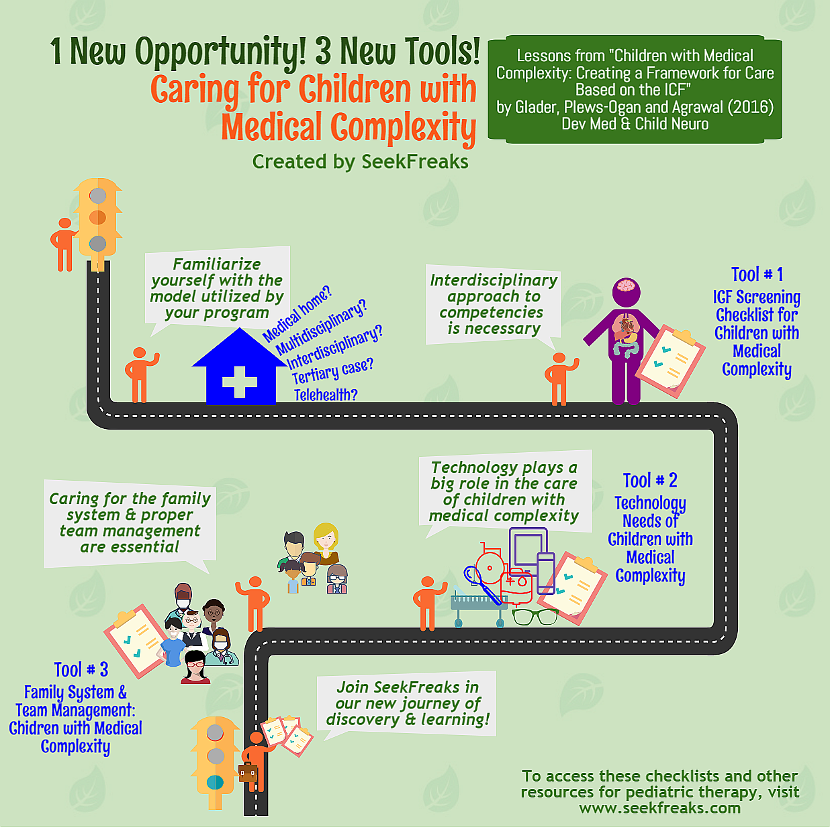
Happy New Year to all SeekFreaks! This new year I have decided to embark on a new challenge; a new opportunity to learn and share newly-found and newly-consolidated knowledge and skills (apologies for using the word ‘new’ 6 times in one short paragraph, but I am quite excited with this development).
Two of the most commonly asked questions at my presentations pertain to the role of therapists working with children with medical complexity (CMC), as well as what therapy assessment & intervention tools are useful for this population. What better way to learn than by doing! So, I decided to take on this challenge by working directly with CMC. This also addresses Resolutions #5 – “Learn something new,” from our 12 SeekFreaks Resolutions for 2017. This year, it is SeekFreaks’ goal to include more discussions around this topic.
I hope you join us in this journey so we can all learn and discover together. To those who already have experience in this area, I look forward to your guidance and support. Join our discussions on our Facebook Group and website. We also invite you to be a SeekFreaks guest contributor and share your expertise with our whole community of learners.
~~~~~~~~~~ 0 ~~~~~~~~~~
I started my learning journey by looking for research in this field. I was glad to find a hot-off-the-press article: Children with medical complexity: creating a framework for care based on the International Classification of Functioning, Disability and Health, by Glader, Plews-Ogan and Agrawal (2016) from the journal, Developmental Medicine& Child Neurology. The authors wrote this article to “develop consistency in approaches to care” for CMC via a proposed framework based on the ICF.
If you have been following us for a while now, you know how muchI love the ICF (Recognizing ICF Domain Words: Amusing Musings). So I quickly dove into this article to extract information and translate them into practice for pediatric OTs, PTs and SLPs.
The article provides many tables that are great summaries of different areas of needs of children and youth with medical complexity. The authors suggested constructing tables based on these, to be “distributed among team members” and “maintained in a patient chart.” We gave these tables a SeekFreaks treatment by turning them into easy-to-use checklists and adding more information, such as those related to school-based practice, which you will find in our discussions below. The authors emphasized that their tables are not exhaustive, so we provide blank spaces on our checklists so you may add other information. You should also feel free to modify the tables to suit your needs.
Here are the main lessons we learned from the article.
1. Familiarize yourself with the model utilized by your program.
- Since multiple disciplines are involved in the care of children and youth with medical complexity, teamwork and collaboration is essential. Thus, it is important to know each member of the team, who leads the team or coordinates the care, and the approach utilized by your program.
- There are 5 general models described in the article. You may notice, as I have, that there are overlaps in their definitions, and programs may include a combination of models.
- Medical Home Model – different disciplines provide family-centered services at home, or in some cases via a hospital-based pediatric practice
- Multdisciplinary Approach – different disciplines with each provider contributing discipline-specific individualized plan of care
- Interdisciplinary Approach – similar to multidisciplinary but with a joint plan of care
- Tertiary Case –placing trained tertiary case nurse practitioners as care coordinators
- Telehealth – providing services remotely, especially where access is an issue
2. Interdisciplinary approach to competencies is necessary.
- A child or youth with medical complexity has broad needs. Team members need to be aware of these. It does not mean that therapists need to be an expert in everything, and assess the child for their every needs. Instead, the authors suggest that the team, as a whole, must ensure that it possesses “team competency” in reviewing and addressing the various needs of the child. This means that there should be a member who is an expert in a particular area of need. The “area expert” must then take the responsibility for regularly assessing and addresses that particular area of need.
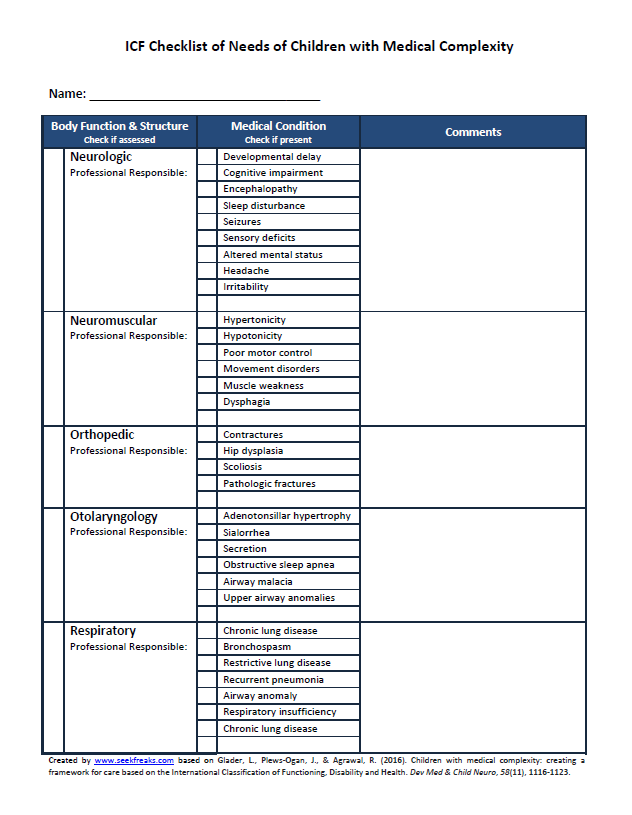
- Neglecting an area of need may be detrimental to the child and the family. So we created a user-friendly ICF Screening Checklist for children and youth with medical complexity based on tables created by the authors. These checklists can make it easier for your team to ensure all areas of need are identified and addressed.
- It is divided among the 5 domains of the ICF: participation, activity, body structure & functions, personal factors and environmental factors. We also included spaces to indicate which team member(s) is/are responsible for regularly screening activity and body structure & function, as specialties come into play in these domains.
- I intentionally started the checklist with the Participation domain to remind continually remind us about the child’s ability to engage as a member of the family, school and community.
Click here to download the full checklist!
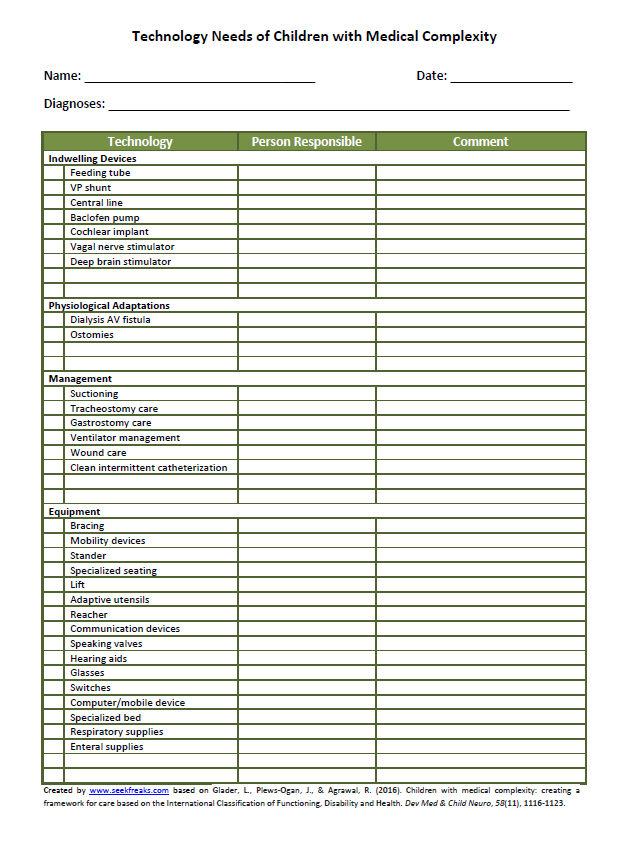
3. Technology plays a big role in the care of Children and Youth with Medical Complexity.
- Various assistive technologies can be great adjuncts to our care, or compensatory strategies to enhance the participation of children and youth with medical complexity in their various social occupations (i.e., as a student, a family member and a member of the community).
- The team needs to be competent in assessing for, selecting and caring for various equipment.
- The authors also emphasized the need to train families and caregivers on use and maintenance of equipment.
- Below is our 2nd checklist (based on a table in the article) to review needs for such equipment. We expanded on the author’s list by adding assistive technology that pertains to areas of OT, PT and SLP.
- We included spaces to indicate the person responsible for the technology.
Click here to download the full checklist!
4. Caring for the family system and proper team management are essential.
- The authors pointed out that caring for children and youth with medical complexity causes significant stress to parents and other caregivers. The caregiver’s own needs and the needs of siblings may be neglected.
- Additionally, the multi-disciplinary teams that work with children and youth with medical complexity require coordination and regular communication.
- Our 3rd checklist, again based on a table from the article, can be a great starting point for reviewing these 2 areas of need. Since the family is an important part of the team, these should be reviewed and shared with the family.
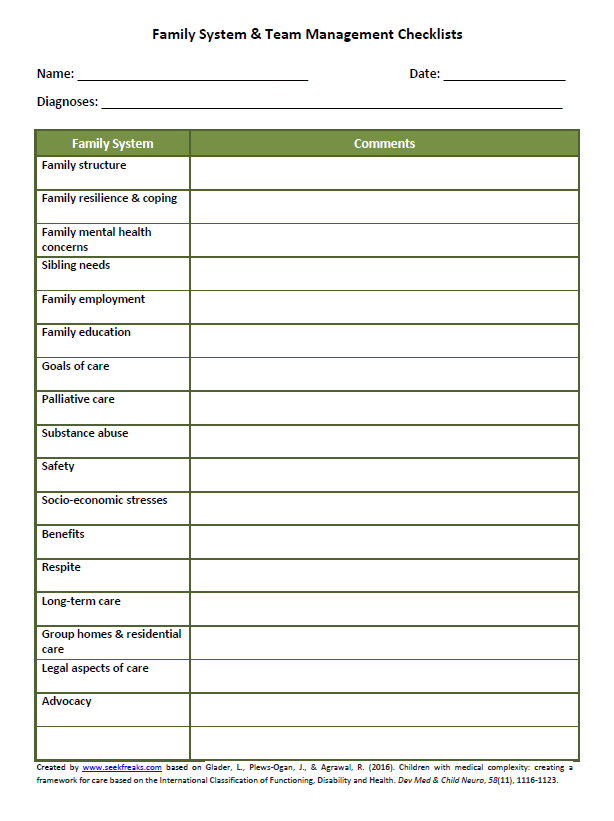 Click here to download the full checklist!
Click here to download the full checklist!
5. Each team member has specific responsibilities.
- As discussed earlier, each team member takes the lead on particular areas of need. The authors created a sample list of responsibilities by each team member (Table IV in the article). We recommend that you review this table.
- We don’t need another checklist for this. The designated spaces for “Professional/Person Responsible” in the 1st 2 checklists above serve the purpose of ensuring that a team member takes the lead in each area.
~~~~~~~~~~ 0 ~~~~~~~~~~
Utility of these Checklists
Most likely your program already uses its own electronic medical record (EMR) system where many of the items in these checklists are already stored. In this case, you may use the checklist as an adjunct to ensure that all possible areas of needs are being reviewed and/or addressed.
The checklists can be used during periodic team meetings to ensure that there is a lead member who is regularly screening for needs in an area that may not currently be identified as a need (e.g., a children and youth with medical complexity does not currently have feeding issues, but a team member should review this area of body function every few months to identify a new need as early as possible). This is especially important if secondary impairments are typical of a particular health condition, and as children get older.
For myself, I like having a checklist with lead persons clearly identified. In case I notice an issue in a particular area, I know who to contact right away. In turn, I would also like my colleagues to know when to contact me so I can stay on top of needs that are under my responsibility.
For those who are creating a new EMR or updating an old one, this checklist is a great tool to incorporate essential items.
SeekFreaks also recommends that you review your state regulations to ensure that you are always in compliance. For example, a state health department may require that all children receiving care under Medicaid or Medicare are assessed by each team member for skin integrity and pain issues every time they provide services. Such requirements can be marked accordingly.
Last but not the least, another great use of these checklists is to provide guidance to SeekFreaks as to the different areas of need we need to research on and discuss in future articles. Once again, if you are an expert in any of these areas, I am sure that other SeekFreaks would love to hear from you. So be a guest contributor, or co-author an article with us. Click here for details on how to become a SeekFreaks guest contributor.
Cheers to the new year and to new opportunities for learning and improving our practice!
~~~~~~~~~~ 0 ~~~~~~~~~~
Readers of this article also read:
2 Tests of Selective Motor Control – SCALE and SCUES
7 Promising Wheelchair Operation Tests
10 Handy American Occupational Therapy Association Fact Sheets