Written by Peggy Morris, OTD, OTR/L, BCP. Peggy is an OT with 30+ years
pediatric experience in early intervention, private practice, and out-patient services – but most of her experience and passion is in school-based practice. She teaches graduate students in the occupational therapy department at Tufts University, and man, do they keep her on her toes! She practices yoga, garden, and play golf for mental health and wellness. She presents evidence-based courses via Apply EBP. More information on these symposiums after the article below.

So this is the thing about evidence:
- we can choose to only use research-based findings,
- we can choose to ignore findings, or
- we can choose to use research findings judiciously
How we react to evidence findings can be a very personal phenomena. Many of us have worked in therapeutic services for all of our professional lives; that professional life can be 30 yrs 🙂 or 2 yrs. For those practitioners on the longer-view end, we have often invested a lot of money into professional development after school finished; those on the shorter-view end have invested an enormous amount of tuition in their newly-minted education. All folks, no matter how long in practice, have an investment in best practice.
Getting back to how we view and ultimately use evidence towards that service of best practice: I often use the analogy of any weight/balance device; think scales of justice. Measuring the evidence with an unbiased eye is a critical professional skill. Published evidence must be analyzed. Not all published studies are well-developed methodologically, not all published studies assist our clinical reasoning with current clients. Some published evidence is well-developed, blows our mind, and makes us think about re-thinking our daily practice routine.
This is also the thing about evidence. For those of us with the longer-view, lots of evidence came after we started working as a therapist! Raise your hand if you graduated therapy school not knowing how to read a research study! (I am raising mine right now).
My BS in OT from 1980 did not prepare me to be an evidence-based practitioner. There was not a lot of evidence for me to use at that time!!!
For those in this longer-view cohort, sometimes reading evidence now makes us think “Yahoo, I have been doing this and it is supported by evidence!” or “Wow, I know this works in my practice, but the evidence doesn’t support it”, or even, “A-ha! I suspected all along this intervention was not working, and now I have evidence that backs me up”. “.
For those of us who have graduated from our therapy education more recently, there is a requirement for you to be taught how to read research, how to analyze strength of research, and how to make a connection between the research and your daily clinical practice – It is a part of your therapeutic identity!
Your challenge is also great; establishing your evidence-based daily practice in the midst of the intervening 10-20 years that its takes evidence to make it into routine care – yes it takes that long to adopt evidence into practice (Burke & Gitlin, 2012; Marr, 2017; Morris et al, 2011).
I guess this is why I started this column in this round-about manner. I wanted to write about a fascinating new research article, it just came into my Twitter feed as folks are starting to read and talk about it globally. And in my world, after two read-throughs, this 2019 article is a landmark, a beacon, and a potential starting or an ending point, depending on where you are in your development as an evidence-based practitioner.
A Landmark Article
This open access article is titled Effectiveness of Paediatric Occupational Therapy for Children with Disabilities: A Systematic Review; authored by Iona Novak and Ingrid Honan, and published in the Australian Journal of Occupational Therapy in 2019; doi: 10.1111/1440-1630.12573
Drs. Novak and Honan have authored a systematic review of 129 systematic reviews and RCTs in pediatric OT; the papers span the years 1935-2016, and include 52 interventions and 22 pediatric disability diagnoses.
The authors of this paper utilized the Cochrane methodology for quality criteria for searching for these studies, the PRISMA statement for reporting, a GRADE format for determining efficacy of the intervention in the study, and an Evidence Alert Traffic Light System (Novak, 2012; Reifenberg & Heinekamp, 2018) as a knowledge translation tool to assist clinicians and families to be able to ‘read’ results easily. These are truly researchers who have done THE heavy lifting for us!
Alright, I want to back up just a bit and detail some of this context. That Cochrane Collaboration is a BIG deal. The Cochrane Library is a collection of high-quality, independent reviews of evidence born to inform healthcare decision-making.
PRISMA
The Cochrane Library houses systematic reviews on topics that are completed by a global panel of experts trained on this type of high-level review. PRISMA stands for Preferred Reporting Items for Systematic Reviews and Meta-Analyses, and Guess What!
Every time we read a published systematic review, we see the PRISMA flow diagram that tells us the number (N = ) of studies found, the number (N = ) that truly answered the research question, the number of studies (N = ) excluded, yada, yada, yada…
GRADE
The GRADE acronym is Grading of Recommendations Assessment, Development and Evaluation that includes a transparent system for grading the quality (or certainty) of evidence and the strength of recommendations that flow from the evidence; GRADE is WHO-endorsed.
Things like rigor of methodology, likely benefits and risks, inconvenience, effect size and the precision of the estimate of that effect size reported in studies, as well as burdens and costs! Phew!
Acronyms give me a headache! But what I’ve realized in sorting this all out is that there is a systematic and transparent process that occurs when reviewers follow best practice in reviewing evidence. And all of this incredible work happens in the background before the authors of systematic reviews can report their findings. This makes me uber-comfortable with this Novak and Honan 2019 article.
The Traffic Light System
One other contextual bit to dig into…the Traffic Light system. Oh, this is gooooood! We all know the traffic light, red, yellow, and green. Red equates to STOP, Green is GO, and Yellow is Caution, right?
Related to its use in EBP,
- Green/Go interventions are those with strong evidence,
- Red/Stop interventions are those with poor strength of evidence or suggests the intervention may be harmful, and
- Yellow/Caution interventions are those with mixed or moderate evidence, that if chosen to be delivered, require outcomes to be closely measured to ensure that data is collected and progress is made with the intervention.
The Review of the Review
Since Novak and Honan reviewed N = 129 studies (N=75 systematic reviews; N= 54 RCTs), I am thinking I cannot fit all of them into this short post, so I’ve picked some of the more well-known interventions to share.
You have really got to head to their bubble chart, it is an ingenious visual support for understanding the BIG picture of the state of pediatric intervention efficacy to date. This bubble chart can really help you to discuss options with your families in your client-centered practice. Alright, diving in!
- Green light for pediatric clients with cerebral palsy:
- If your client has cerebral palsy and you are interested in motor outcomes of intervention, CIMT (constraint-induced manual therapy) is a Green/Go, it has the biggest bubble strength of evidence.
- Bimanual training is also a Green/Go. In a closer look at these studies, the clients who benefit are those with cerebral palsy, hemiparesis type. I’ve read the research in both of these areas, so I know these two approaches, and, man do they benefit!
- Goal-directed training for motor outcomes in clients with cerebral palsy is also a Green/Go intervention. I actually do not know as much about goal-directed training as I evidently should, given its high rating on efficacy, so I headed into GoogleScholar to see what I could find to inform me. I found that goal-directed training is a top-down, occupation-based approach to intervention that relies on the client identifying the goal, establishing baseline performance of that goal (not necessarily the underlying sensorimotor foundations we might assume to be involved), an intervention/practice phase, and then progress monitoring.
- Because I stepped into new literature, I found that I am intrigued by this intervention possibility. I do know the literature on the efficacy of coaching (also big Green/Go bubble under the Parent Outcome in this review), and I’m feeling this goal-directed training appears at first blush to pair nicely with coaching evidence-based practice. Hmmm…the power of combining two evidence-based interventions? I’m interested in figuring this out! Hmm, I’ve been led somewhere new! Nervous, but excited about how this might change my practice!
- Ok, so here is the less-than-comfortable part: NDT is recommended as a Red/Stop intervention for motor outcomes for clients with cerebral palsy.
- What this systematic review is offering me and my clinical reasoning is that NDT is less supported by strong evidence than at least three other intervention options.
- I can be pissed, I can be defensive, I can be open. I can be lots of other things when I read this part of the article; again, our reactions to evidence can be very personal. Initially, my personal reaction has usually been “OK, hmm, don’t really like this information, ‘cause I was taught about NDT in school (‘member, I’m in the long-view group) and I’ve spent money on professional development in this area.”
- Change is uncomfortable; I am not the first person to grapple with this! With some reflection and time, I find change is also a wonderful opportunity to re-assess skills, values, beliefs, new ideas, old ideas. Change happens whether we are into it or not. I actually remember when there were no children on the spectrum in my workload! (long-view, old OT here!). That has certainly changed, and I feel the need to continuously update my knowledge and skills because I did NOT learn about autism in OT school. As practice morphs and the ground beneath us shifts, we can be off-kilter, off-balance. Un-comfortable to say the least.
- Interventions for pediatric clients with DCD:
- OK, back to the article. I am going to stick with motor as outcomes of intervention for now. If your client has a diagnosis of DCD, then the CO-OP method is Green/Go! Ah, I LOVE the CO-OP method. Goal-Plan-Do-Check, a very top-down, occupation-based approach.
- In terms of a handwriting motor outcome for clients with DCD, handwriting task practice is a Green/Go intervention.
- The related Red/Stop intervention for clients with DCD is a sensory approach to handwriting.
- What this is offering me and my clinical reasoning is the knowledge that practicing handwriting is more efficacious than a sensorimotor approach to handwriting. While this may also be tricky to embrace, I am thankful for the researchers adding this nugget of wisdom to my clinical reasoning bag o’ tricks.
- Can we try one more population and dip into understanding the Yellow range of the traffic light?
- For behavioral outcomes with the ASD population, meditation is supported in the Yellow/Caution range.
- Interestingly, these authors have placed a “worth it” ——- line on their graphic, to denote
- the Yellow/Caution interventions that are W+, worth it, probably do it
- and those Yellow/Caution interventions that are W-, not worth it, probably don’t do it.
- So meditation is above the worth it line, in the W+ range. When we use an intervention from the Yellow/Caution range of effectiveness, it’s even more important that we must complement that with a data collection system to measure the outcome for our particular client; data collection is how we make individualized evidence.
- There is another intervention in the behavioral outcomes for clients with ASD that is Yellow/Caution, but floats below the “worth it” line at W-, sensory approaches (differentiated from sensory integration). Again, what this affords my clinical reasoning is that I have choices! And who does not love choices! For more on EBP in ASD, check out a previous SeekFreaks post.
- The trend of what’s more likely to be Green than Red:
- There are other outcomes and conditions represented in the bubble visual, but I am getting close to the finish of this post.
- Outcomes included behavior, pain, feeding, cognition, sleep, mental health and a few others.
- Pediatric conditions included cerebral palsy, ASD, Down syndrome, burns, ADHD, brain injury, DCD, and more.
- And a brain-blower result from this systematic review: a trend in the intervention results favoring top-down, occupation-based interventions was observed in the data.
- I want to say that again, but in a slightly different way: in this systematic review of systematic reviews and RCTs, interventions that were targeted at the participation/occupation level and at the activities level tended toward more effectiveness than interventions targeted at the body structures and function level (there is also a really nice graphic about this in the article as well).
The Learning Continues…Summer Reading
OK, summer reading recommendation/challenge, if you are interested. This article identifies 39 effective evidence-based pediatric interventions that exist today.
I invite you to download this article, read it at least twice, mark it up with a highlighter and sticky tabs J, and wonder.
Marvel at the hard work of the authors. Be grateful for their translating a ton of research into a very palatable article and an unbelievably clear visual support. Be curious, be a scientist, be an advocate for the best intervention for each and every client you serve.
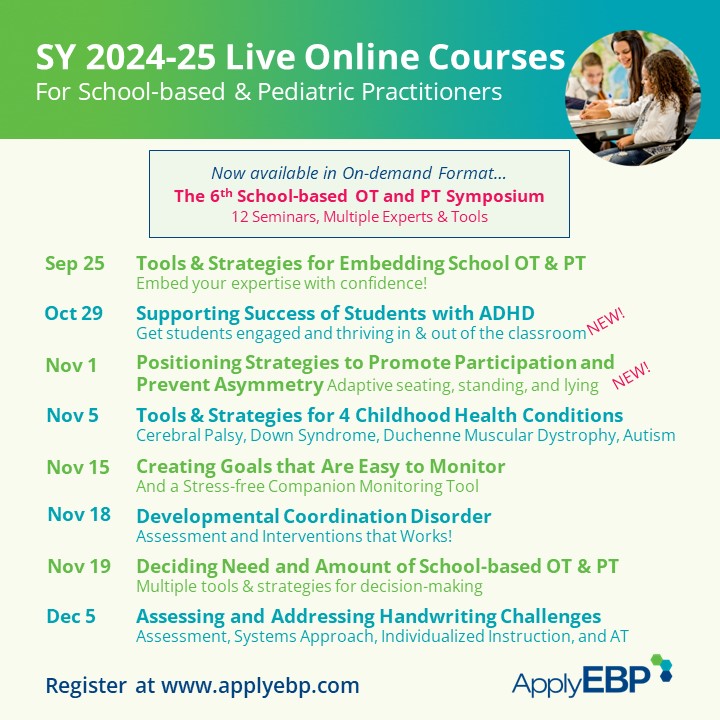
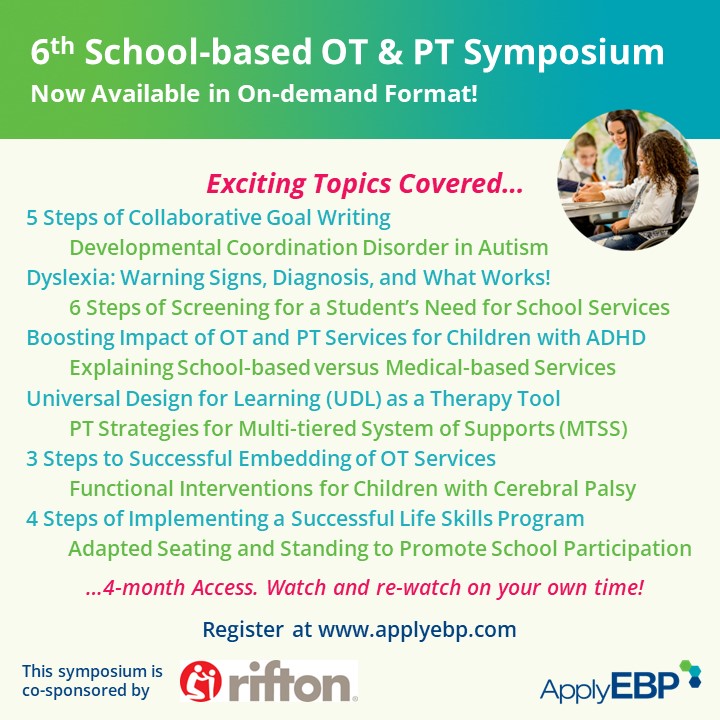
Join Peggy and other evidence-based presenter at these courses…
References
Burke, J. P., & Gitlin, L. N. (2012). How do we change practice when we have the evidence? American Journal of Occupational Therapy, 66(5), e85-e88.
Marr, D. (2017). Fostering Full Implementation of Evidence-Based Practice. American Journal of Occupational Therapy, 71(1), 7101100050p1-7101100050p5.
Morris, Z. S., Wooding, S., & Grant, J. (2011). The answer is 17 years, what is the question: understanding time lags in translational research. Journal of the Royal Society of Medicine, 104(12), 510-520.
Novak, I. (2012). Evidence to practice commentary: the evidence alert traffic light grading system. Physical & occupational therapy in pediatrics, 32(3), 256-259.
Novak, I., & Honan, I. (2019). Effectiveness of paediatric occupational therapy for children with disabilities: A systematic review. Australian occupational therapy journal. doi: 10.1111/1440-1630.12573
Reifenberg, G, & Heinekamp, A. (2018). Using the traffic light system to implement evidence-based practice. OT Practice, 23 (20), 28-31.









June 24, 2019 at 2:55 pm
Hello there! Quick question that’s entirely off topic.
Do you know how to make your site mobile friendly? My website looks weird when browsing from my iphone4.
I’m trying to find a theme or plugin that might be able to fix this
issue. If you have any suggestions, please share.
Many thanks!