Carlo Vialu, PT, MBA, is co-creator of SeekFreaks. He loves promoting function and participation for children and youth with disabilities, from our assessment to our interventions, via his continuing education platform, Apply EBP. Read more about these courses after the article.
What you will learn from this article…
- How good are we at practicing the evidence?
- What interventions work?
- How do I apply these when providing services online?
- How do I know if my online interventions are informed by evidence?
- Will evidence-based practices be one of the casualties of the pandemic?
Therapy in the time of the pandemic…
The most common question I have been getting from SeekFreaks and Apply EBP followers is: What interventions work online, instead of face-to-face?
Surely, the current pandemic has shaken the way we provide services, whether you are providing services online, or in-person but with lots of safety precautions, including wearing personal protective equipment (PPE), handwashing and frequent sanitizing.
There are no conclusive research about therapeutic interventions provided online. But, the answer to the question of what interventions we should be doing now, remains the same: the evidence of what works has not changed…just the way we deliver the service!
As pediatric therapists, we have been gifted in the past 2 years with lots of systematic reviews and guidelines where the authors have done the heavy lifting (to quote Peggy Morris) so that we know interventions that work and those that do not.
As recipients of these gifts of research, and as science practitioners, our duty to our clients is to apply these evidence to promote successful outcomes!
How Good Are We at Practicing Based on Evidence?
Before we look at those evidence, let’s see how good we have been at following the evidence.
Peggy Morris, OTD, OTR/L, BCP called my attention to this study by Piller and Torrez (2019). They examined narrative notes to look at what interventions 157 occupational therapists provided to 5-15 year-old children with handwriting difficulties. They found the following distribution of interventions:
- Multi-sensory/Sensorimotor: 27%
- Motor/Kinesthetic: 27%
- Cognitive: 19%
- Therapeutic Practice: 18%
- Task-oriented: 9%
If you are an OT practitioner, and somebody were to review your documentation in the past week (for addressing handwriting difficulties), what percentage of each of the above would they find?
Contrast that with the conclusion of the latest systematic review about handwriting interventions. This is what Grajo et al (2020) reported about their effectiveness:
- They found moderate evidence to support these interventions for improving handwriting legibility:
- Therapeutic practice
- Cognitive strategies
- Provision of performance feedback
- Evidence show these have no effect on handwriting legibility for sensorimotor handwriting interventions that address isolated component skills, such as
- visual perception
- kinesthesia
- in-hand manipulation
- visual–motor integration
- biomechanical features of handwriting
Similar findings were reported by Novak and Honan (2019), Blank et al (2019), and Fancher et al (2018), among others.
Did the misalignment of current practice to evidence surprise you?
While there is no equivalent study for pediatric physical therapists, Zadro et al (2019), found in their systematic review of physical therapy for musculoskeletal conditions that:
- In 23 studies, when asked, 54% of therapists chose recommended treatments (survey studies)
- In 8 studies, when documentation is reviewed, 63% of patients received recommended PT-delivered treatments (audit studies)
I was floored by the above numbers. At best, only 4 to 6 out of 10 times do therapists in the studies above provide or recommended interventions that are supported by evidence.
Which also means the opposite, that 4 out of 6 times out of 10, therapy clients may not be receiving interventions that are supported by evidence.
So What Interventions Work?
For more detailed information, I recommend that you read the systematic reviews in the list at the end of this article. There is so much evidence, that I will not try to fit them all in this article.
What I will report to you instead are the themes that authors have found with regards to interventions that work:
- Blank et al (2019), supports the use of task-oriented approaches for children with DCD. Here are the “mandatory characteristics of task‐oriented or activity‐oriented interventions:
- client‐oriented (meaningful for the client)
- goal‐oriented (aiming at activities and participation as described in the Children and Youth Version of the ICF)
- task and context specific (what is to be learned, and for which circumstances)
- those that consider the client to take an active role
- aiming at functionality, not at normality
- active involvement of parent(s)/caretakers to enable transfer.”
- Novak and Honan (2019), reports green light or GO for “top-down” activity level interventions with “the following key ingredients in common:
- begin with the child’s goal, to optimize motivation and saliency of practice;
- practice of real-life activities in natural environments to optimise the child’s learning and the variability of the practice;
- intense repetitions to activate plasticity, including home-based practice; and
- scaffolded practice to the ‘just right challenge’ to enable success under self-generated problem-solving conditions, to optimise enjoyment.”
- Cahill and Beisber (2020), in their OT Practice Guidelines for Children and Youth Ages 5-12 years old in AJOT recommend that OT practitioners:
- Consistently collaborate with families and caregivers
- Provide services in the natural context of the desired occupation
- Group service models/models that include peer mediation to promote participation
- Skills-based training and therapeutic practice in the context of the valued occupation
I can go on and on but let me not bore you. Hopefully you are already seeing a pattern here of what works.
How Do I Apply This When Providing Services Online?
Just like anything that is new, if you have not provided services online before, it can be scary and downright frustrating. In the frenzy of figuring out what we can do, we search online for interventions, or we ask others for recommendations.
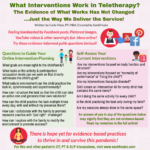
Even without searching, we are bombarded by creative Facebook posts, Pinterest images, YouTube videos, product commercials and continuing education of things that therapists can do online. And we Oooohhh or Aaaahhhh, as we think about how to re-create them during our 30 minutes or so online.
But alas, all that glitters is not gold! In my years as a therapist, I have seen treatment fads (that are not supported by evidence) come and go, and fads that linger, or come bubbling back up every so often.
What excites me about what I listed above as key ingredients for what works is that they are doable in services delivered online! Don’t you agree?
- Work on the goal of the child…check, I can do that!
- Work on meaningful tasks at the activity and participation level…check that too!
- Collaborate with the family….check again!
- Practice in the natural environment…they’re at home, not in a made-up environment, so check!
- And on and on…
I am not saying it would be easy, or that there are no barriers to doing any of the above. Surely there are, similar to there being barriers in any setting. But the potential is there to apply the evidence in online services!
So, instead of going with the fad, I will provide you with some questions based on the key ingredients listed above that will hopefully guide you when you are planning your interventions online:
- What goals are meaningful to the child and the family?
- What tasks at the activity and participation/occupation levels can we work on that directly addresses the child’s goal?
- What natural environment can the child practice the task in?
- Can this be done synchronously with me online with the child?
- If not, can I coach the child and the family to perform the task in the natural environment asynchronously?
- How can I structure the task so that the child can take an active role and generate their own solutions?
- How can the child practice the task multiple times every day, with and without my presence there?
- How can I collaborate with the family to promote repeated practice with just the right amount of challenge?
- How can I collaborate with the family to modify the environment to promote success?
How Do I Know If My Online Interventions Are Informed by Evidence?
Many of us have already started providing services online. So I created these questions so you can self-assess whether your interventions follow the evidence.
An answer of yes to any of the questions below may signify that they are not evidence-based. So I provide suggestions to make them so…they just need a little tweaking!
- Are my interventions focused on body function and structure? (e.g., visual perception, fine motor, strengthening, range of motion)
- Bump up your interventions into the activities and participation/occupation levels. Think meaningful verbs like walking, writing, talking, dressing, handwashing! What school activity can they complete instead of sorting mini-pom-poms or doing mazes online? What chores can they complete at home that would require their strength to lift and squat?
- Are my interventions focused on “normality of performance” or “fixing the child”?
- Focus instead on function. Modify the environment or guide the child with questions so they can self-generate solutions on how they can use their body to complete the task successfully, in a way that their body allows them to do.
- Are my interventions therapist-directed?
- If you find yourself talking too much or telling them what they need to do, ask more questions instead. Help the child/family come up with their own goals, explore different plans, and self-monitor their own progress.
- Did you create an intervention kit for every child that contains the same items?
- This may be a sign that your interventions are not individualized. Have the child/family explore what to put in their own kit. What items are meaningful to them? What tools can help them reach their goals?
- Are you doing the same activity for every child?
- This may be another sign that your interventions are not individualized. Review the child’s goals and come up with activities that are in line with those goals.
- Is the child practicing the task only during your session?
- Find a task that is meaningful to the child and family so they will work on it even if you are not around. Work with the child and family to find lots of opportunities for practice throughout the day, every day of the week.
- Are your “sessions” always occurring in the same space?
- This one may be tough to remedy for some home setup. But thinking about the natural environment, can you bring it to the kitchen for some meal prep? To the laundry room? Outside? If you can’t do any of the above, can you coach the family to bring the activities to different, more natural environment when you are not around?
Will Evidence-based Practices Be One of the Casualties of the Pandemic?
Truth be told, when our services moved online because of the pandemic, I saw the following pros: I thought that we can see what children really do at home and what is meaningful to them and their families. That in doing so, we can figure out activities that can be better carried over into their daily lives. More practice, yay! And that we are able to collaborate more with parents and caregivers.
But I also thought of the cons: that those of us who have already learned to embed ourselves in the classroom or at home, will end up working in isolation with the child again within the un-natural environment of sitting right across from each other in front of a computer. I thought that we might be providing interventions that are easy to do online, but not evidence-based. Mostly, I was afraid that we bring these interventions back to our in-person services once the pandemic is over.
While the latter has come true, I still want to see the positive side of what’s happening. So I posted a survey on a Facebook Group page for school-based OTs and PTs and asked about the positives they got from doing teletherapy. And here are the answers based on number of votes:
- I was able to work on carryover of activities with family – 156 votes
- I learned that I can effective being “brains on”, since “hands on” is not an option – 111 votes
- I learned the home situation and how I can support it – 95 votes
- I found out what the family’s need and goals are – 43 votes
- I was able to strengthen my relationship with the family – 39 votes
- I was able to educate families, helped them developed a greater understanding for the “why” – 32 votes
- I learned the family routine – 32 votes
- I will have more input for the child for the next IEP meeting – 31 votes
- I learned what the child is really interested in – 29 votes
- I learned about what works, what is not working, engagement in problem solving – 23 votes
These responses made my EBP heart leap. There is hope yet for evidence-based practices to thrive in and survive this pandemic!
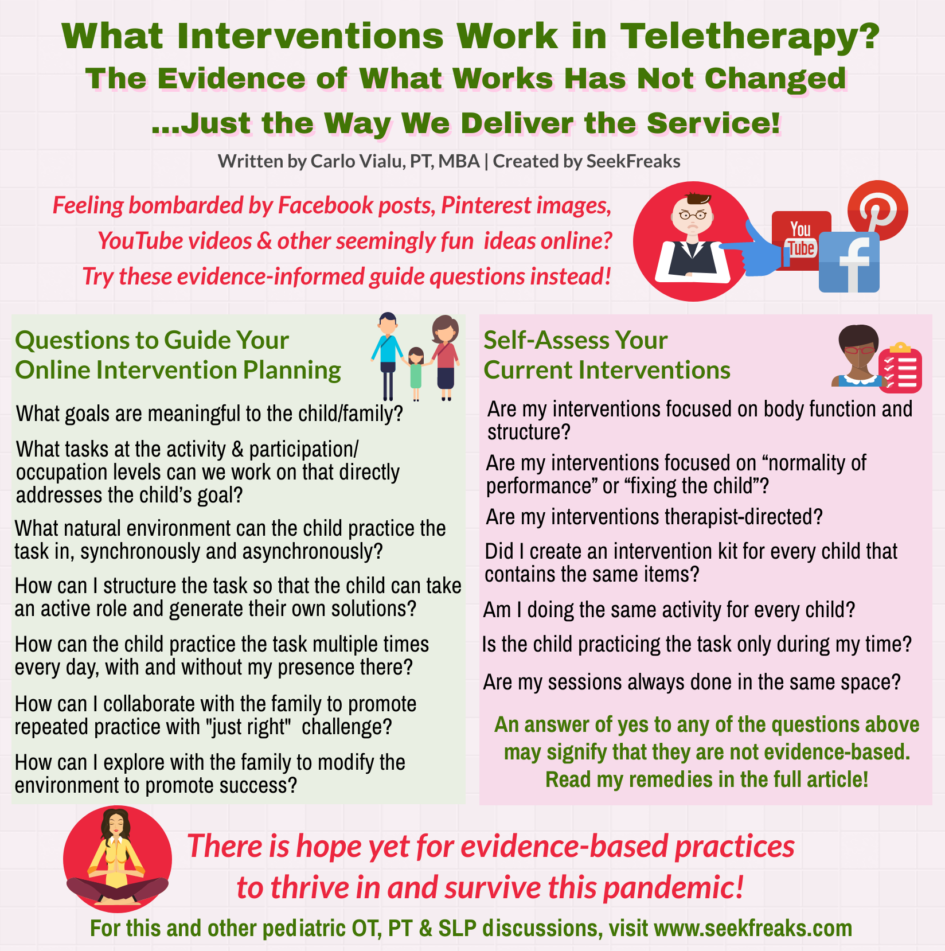
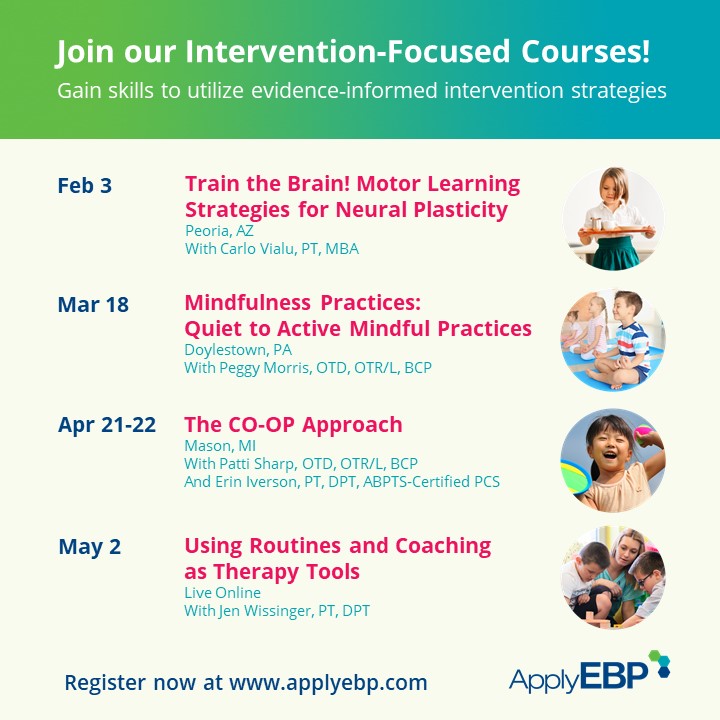
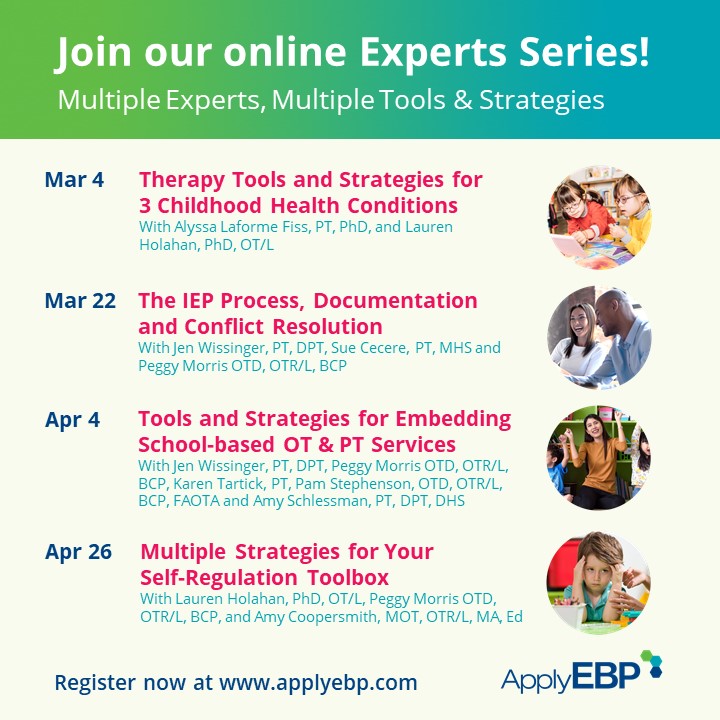
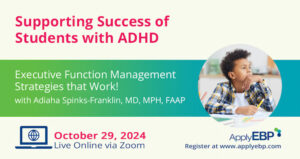
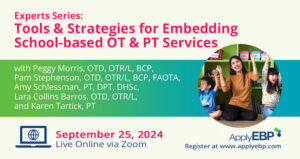
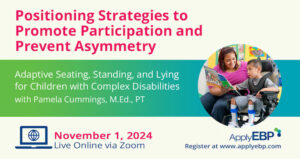
Join Carlo Vialu and other experts at these all evidence-based, all practical continuing education courses:
Systematic Review/Guideline Must-Reads
- Blank, R., Barnett, A. L., Cairney, J., Green, D., Kirby, A., Polatajko, H., … & Vinçon, S. (2019). International clinical practice recommendations on the definition, diagnosis, assessment, intervention, and psychosocial aspects of developmental coordination disorder. Developmental Medicine & Child Neurology, 61(3), 242-285.
- Cahill, S. M., & Beisbier, S. (2020). Occupational Therapy Practice Guidelines for Children and Youth Ages 5–21 Years. American Journal of Occupational Therapy, 74(4), 7404397010p1-7404397010p48.
- Grajo, L. C., Candler, C., & Sarafian, A. (2020). Interventions Within the Scope of Occupational Therapy to Improve Children’s Academic Participation: A Systematic Review. American Journal of Occupational Therapy, 74(2), 7402180030p1-7402180030p32.
- Novak, I., & Honan, I. (2019). Effectiveness of paediatric occupational therapy for children with disabilities: A systematic review. Australian occupational therapy journal, 66(3), 258-273.
- Novak, I., Morgan, C., Fahey, M., Finch-Edmondson, M., Galea, C., Hines, A., … & Shore, B. (2020). State of the evidence traffic lights 2019: systematic review of interventions for preventing and treating children with cerebral palsy. Current neurology and neuroscience reports, 20(2), 1-21.
- Tanner, K., Schmidt, E., Martin, K., & Bassi, M. (2020). Interventions within the scope of occupational therapy practice to improve motor performance for children ages 0–5 years: A systematic review. American Journal of Occupational Therapy, 74(2), 7402180060p1-7402180060p40.
Additional References
- Piller, A., & Torrez, E. (2019). Defining occupational therapy interventions for children with fine motor and handwriting difficulties. Journal of Occupational Therapy, Schools, & Early Intervention, 12(2), 210-224.
- Zadro, J., O’Keeffe, M., & Maher, C. (2019). Do physical therapists follow evidence-based guidelines when managing musculoskeletal conditions? Systematic review. BMJ open, 9(10), e032329.









August 20, 2020 at 6:01 pm
It was helpful. Thank you!
August 28, 2020 at 3:48 pm
Thank you Carlo! I love the words you used “ all that glitters is not gold”
I think the remote work with students and families is helpful for all. Practice, repetition, interests, and kisC keeping it simple yet challenging .. that just right challenge.
Thinking “ playing with dolls” trucks/ cars
Best to all.
September 4, 2020 at 7:12 am
Great article. thanks much. I have seen suggestions for some PT activities via Teletherapy that seem quite popular but mostly involve exercise in a contrived way as opposed to functional activities within the home. We need to become much more creative in this regard and remember that we can embed all kinds of therapeutic activities in the daily home or in-school routine.